In vitro antibacterial activity of Acorus calamus extract on methicillin-resistant Staphylococcus aureus wound isolates and reduced invasion into mucosal fibroblasts
Research Articles | Published: 12 October, 2020
First Page: 712
Last Page: 721
Views: 3817
Keywords: Acorus calamus , Methicillin-resistant Staphylococcus aureus (MRSA), Antibacterial activity, Bacterial invasion, Phytochemical analysis, Mucosal fibroblasts
Abstract
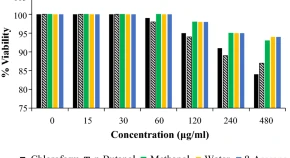
Acorus calamus is widely used as an Indian medicinal plant and extensively reported for treatments of skin, digestive and nervous disorders. A methanol extract of A. calamus (rhizome) showed maximum extraction yield of 4% (w/w) followed by 3% (w/w) in water. Total 8 Staphylococcus aureus isolates were obtained from nose, groin, wounds, axilla, throat of various patients exhibited strong β-lactamase activity and antibiotic resistance for ampicillin, oxacillin, and methicillin coded for mec A gene. Thus, all isolates belong to methicillin-resistant Staphylococcus aureus (MRSA) class. Methanol extract is the most potent MRSA antibacterial extract followed by water, n-butanol and chloroform. Minimum inhibitory concentration (MIC) of methanol extract varied from 1.25 to 2.50 mg/ml for all MRSA isolates which also exhibited highest MIC values of 512 µg/ml and 128 µg/ml for ampicillin and oxacillin antibiotics, respectively. Interestingly, the synergistic interaction of 128 µg/ml of A. calamus methanol extract with antibiotics (ampicillin, 64 µg/ml and oxacillin, 32 µg/ml) showed lowered MICs. All extracts of A. calamus and β-asarone showed no significant cytotoxic activity against non-cancerous 3T3 fibroblasts cells which was confirmed by MTT assay on MRSA-08 isolate. Antibacterial effect and preventive invasion properties of MRSA of methanol extract of A. calamus were found to be potent when compared with β-asarone, an active component of A. calamus. The present investigation showed a correlation of polyphenolics and flavonoid based major phytochemical constituents with bioactivities on MRSA revealed A. calamus as a potential non-toxic drug candidate for various skin diseases.
References
- Adhikari R, Pant ND, Neupane S et al (2017) Detection of methicillin resistant Staphylococcus aureus and determination of minimum inhibitory concentration of vancomycin for Staphylococcus aureus isolated from pus/wound swab samples of the patients attending a tertiary care hospital in Kathmandu, Nepal. Can J Infect Dis Med Microbiol 2017:1–6. https://doi.org/10.1155/2017/2191532
- Ali S, Khan MR et al (2018) Phytochemical investigation and antimicrobial appraisal of Parrotiopsis jacquemontiana (Decne) Rehder. BMC Complement Altern Med 18:43. https://doi.org/10.1186/s12906-018-2114-z
- Almeida RA, Matthews KR, Cifrian E et al (1996) Staphylococcus aureus invasion of bovine mammary epithelial cells. J Dairy Sci 79:1021–1026. https://doi.org/10.3168/jds.S0022-0302(96)76454-8
- Aqil F, Ahmad I, Owais M (2006) Evaluation of anti-methicillin-resistant Staphylococcus aureus (MRSA) activity and synergy of some bioactive plant extracts. Biotechnol J 1:1093–1102. https://doi.org/10.1002/biot.200600130
- Archana SN, Pant AK, Prakash O (2015) Acorus calamus (Sweet flag): a medicinally important plant. Int J Inst Pharm Life Sci 5:232–240
- Asha DS, Ganjewala D (2009) Antimicrobial activity of Acorus calamus (L.) rhizome and leaf extract. Acta Biol Szeged 53:45–49
- Bahukhandi A, Rawat S, Jugran AK et al (2020) Seasonal variation in phenolics and antioxidant activity of Acorus calamus Linn.: an important medicinal plant of Himalaya. Natl Acad Sci Lett. https://doi.org/10.1007/s40009-020-00959-3
- Balakumbahan R, Rajamani K, Kumanan K (2010) Acorus calamus: an overview. J Med Plants Res 4:2740–2745
- Chang SC, Chen YC, Luh KT, Hsieh WC (1995) In vitro activites of antimicrobial agents, alone and in combination, against Acinetobacter baumannii isolated from blood. Diagn Microbiol Infect Dis 23:105–110. https://doi.org/10.1016/0732-8893(95)00170-0
- Chaudhri RD (1996) Herbal drug industry: a practical approach to industrial pharmacognosy, 1st edn. Eastern Publishers, New Delhi
- Chew YL, Mahadi AM, Wong KM, Goh JK (2018) Anti-methicillin-resistance Staphylococcus aureus (MRSA) compounds from Bauhinia kockiana Korth. And their mechanism of antibacterial activity. BMC Complement Altern Med 18:70. https://doi.org/10.1186/s12906-018-2137-5
- Davies J, Davies D (2010) Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev 74:417–433. https://doi.org/10.1128/MMBR.00016-10
- Gordon RJ, Lowy FD (2008) Pathogenesis of methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis 46:S350–S359. https://doi.org/10.1086/533591
- Heyman HM, Hussein AA, Meyer JJM, Lall N (2009) Antibacterial activity of South African medicinal plants against methicillin resistant Staphylococcus aureus. Pharm Biol 47:67–71. https://doi.org/10.1080/13880200802434096
- Kali A (2015) Antibiotics and bioactive natural products in treatment of methicillin resistant Staphylococcus aureus: a brief review. Pharmacogn Rev 9:29. https://doi.org/10.4103/0973-7847.156329
- Khwairakpam AD, Damayenti YD, Deka A et al (2018) Acorus calamus: a bio-reserve of medicinal values. J Basic Clin Physiol Pharmacol 29:107–122. https://doi.org/10.1515/jbcpp-2016-0132
- Kim H, Han TH, Lee SG (2009) Anti-inflammatory activity of a water extract of Acorus calamus L. leaves on keratinocyte HaCaT cells. J Ethnopharmacol 122:149–156. https://doi.org/10.1016/j.jep.2008.12.011
- Kumar S (2016) Studies on antioxidant and antimicrobial activity of Acorus calamus and Myristica fragrans. Int J Appl Res 2:292–297
- Marlowe EM, Bankowski MJ (2011) Conventional and molecular methods for the detection of methicillin-resistant Staphylococcus aureus. J Clin Microbiol 49:S53–S56. https://doi.org/10.1128/JCM.00791-11
- McGaw LJ, Jäger AK, van Staden J, Eloff JN (2002) Isolation of β-asarone, an antibacterial and anthelmintic compound, from Acorus calamus in South Africa. S Afr J Bot 68:31–35. https://doi.org/10.1016/S0254-6299(16)30450-1
- National Medicinal Plants Board (2008) Agro-techniques of selected medicinal plants. TERI Press, New Delhi
- NCCLS (1995) Performance standards for antimicrobial susceptibility testing. Sixth informational supplement, Villanova
- Okwu MU, Okorie TG, Agba MI et al (2014) Comparative anti-MRSA activities of seven selected Nigerian medicinal plants and phytochemical constituents of Piper guineense (Schum and Thonn.), Curculigo pilosa (Schum and Thonn.) and Chromolaena odorata (King and Robinson). IOSR J Pharm Biol Sci 9:7–13
- Phongpaichit S, Pujenjob NVR, Ongsakul, and M, (2005) Antimicrobial activities of the crude methanol extract of Acorus calamus Linn. Songklanakarin J Sci Technol 27:517–523
- Rajput SB, Tonge MB, Karuppayil SM (2014) An overview on traditional uses and pharmacological profile of Acorus calamus Linn. (Sweet flag) and other Acorus species. Phytomedicine 21:268–276. https://doi.org/10.1016/j.phymed.2013.09.020
- Ramos-Ocampo VE, Hsia MTS (1988) Mutagenic and DNA-damaging activity of calamus oil, asarone isomers and dimethoxypropenylbenzenes analogues. Philipp Entomol 7:275–291
- Rochon-Edouard S, Pestel-Caron M, Lemeland J-F, Caron F (2000) In vitro synergistic effects of double and triple combinations of beta-lactams, vancomycin, and netilmicin against methicillin-resistant Staphylococcus aureus strains. Antimicrob Agents Chemother 44:3055–3060. https://doi.org/10.1128/AAC.44.11.3055-3060.2000
- Shahzad N, Alam A, Sultana N, Asma K (2015) Phytochemical and pharmacological studies of Vaj Turki (Acorus calamus Linn.) & Unani description—a review. Int J Pharma Sci Res 6:1241–1244
- Shibata H, Kondo K, Katsuyama R et al (2005) Alkyl gallates, intensifiers of β-lactam susceptibility in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 49:549–555. https://doi.org/10.1128/AAC.49.2.549-555.2005
- Shreelaxmi MP, Sharanagouda H, Ramachandra CT et al (2017) Supercritical fluid extraction of oil from sweet flag rhizome (Acorus calamus L.) and its insecticidal activity on pulse beetles (Callosobruchus maculatus). Int J Curr Microbiol Appl Sci 6:3608–3615
- Subha T, Gnanamani A, Mandal A (2011) Pharamcognostic evaluation of Acorus calamus L. Pharmacogn J 3:24–27. https://doi.org/10.5530/pj.2011.23.4
- Umamaheshwari N, Rekha A (2018) Sweet flag: (Acorus calamus)—an incredible medicinal herb. J Pharmacogn Phytochem 7:15–22
- Vajrabhaya L, Korsuwannawong S (2018) Cytotoxicity evaluation of a Thai herb using tetrazolium (MTT) and sulforhodamine B (SRB) assays. J Anal Sci Technol 9:15. https://doi.org/10.1186/s40543-018-0146-0
- WHO (2000) General Guidelines for Methodologies on Research and Evaluation of Traditional Medicine. World Health Organization, Geneva
- Zambare VP (2009) Antibiotic resistance and sensitivity pattern of pathogenic bacteria isolated from urinary tract infected sample. Biomed Pharmacol J 2:137–140
- Zhao WH, Hu ZQ, Okubo S et al (2001) Mechanism of synergy between epigallocatechin gallate and β-lactams against methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 45:1737–1742. https://doi.org/10.1128/AAC.45.6.1737-1742.2001
- Zuo GY, Zhang XJ, Yang CX et al (2012) Evaluation of traditional Chinese Medicinal plants for anti-MRSA activity with reference to the treatment record of infectious diseases. Molecules 17:2955–2967. https://doi.org/10.3390/molecules17032955
Author Information
Smt. Chandibai Himathmal Mansukhani College, Ulhasnagar, India